by Dr. Nicholas J Lelos
“Those that fail to learn from history are doomed to repeat it” Winston Churchill
The historical perspective, before the current analysis.
There have been several infections afflicting mankind over its chequered history.
Nomenclature and definitions first: an epidemic is a surge and spread of a disease to a large number of people, usually in a specific area over a short period of time. The word itself derives from a notion attributed to the Odyssey from Homer, then becoming a medical term in a treatise by Hippocrates – translating as “upon or above “ and “people”. Endemic in contrast, is used to refer to a disease that is present at low rates in a population.
Once the disease spreads to a certain percentage of population or spreads geographically crosses borders, it is described a pandemic.
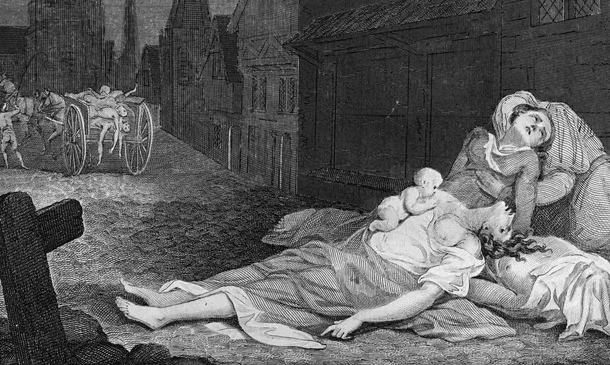
The Plague is an example.
So is the Spanish Flu, which ironically is first observed in the United States but as the media were censored in fully reporting on it due to the First World War, it was more described in Spain. This gave the impression that the country was particularly affected and the moniker “Spanish Flu” came about.
This particular strain of influenza, of the H1N1 variety, proved to be particularly virulent – no less than 4 waves around the world were documented, with an estimated 500 million infections.
The circumstances compared with now were slightly different – the end of World War 1, large movements of troops, poor nutrition, rationing, wounds and other illnesses contributed heavily. It became a ‘blitz’ pandemic, compared to the Black Plague in the Middle Ages, which lasted for several years longer, and killed a larger percentage of the global population.
Due to the lack of the right technology and knowledge, vaccines for influenza type A and B were developed only in 1938.
Till then, what curbed the infection, was surprisingly similar to what is happening currently – distancing, closing of businesses, advice about covering coughs, wearing of masks, washing hands and curfews to reduce numbers of people up and about, business and entertainment suffered – the pandemic receded, and we now see that strain still as the seasonal flu.
Partially due to the knowledge we gained in public health measures, hygiene, as well as the annual vaccination programs of various countries to provide protection to the most vulnerable citizens.
Fast-forward 102 years to COVID-19.
COVID-19 is on the global stage. Efforts to produce a vaccine, which had already begun since the SARS and MERS strains, are now in full swing, with more money and coordinated efforts than ever before.
Many countries are in a travel lockdown, with some societies being grid-locked in curfews and lockdowns, others, such as Australia, having their borders nigh-on shut.
It is worthy of notice that his has been the most united research and development effort for solutions to this strain that many other pharmaceutical research projects.
It also pushed the boundaries for the development of many exciting and hitherto untried techniques and approaches.
This, of course, also has the consequence that a lot of the treatments are ground-breaking and that data is continuously coming out, with more information gained daily about their efficiency and effectiveness.
Now, a general note about virus vaccines
Previous technologies relied on providing either a live-but-inactive version of the virus, a weakened one, or of constituents of the virus – little pieces.
The aim is to get the immune system of the recipient to identify the trespasser, and next time it sets foot in the body the immune system is on high alert and has defence mechanisms activated and ready to pounce on the invader.
This has worked on several deadly viruses such as smallpox and polio (strain 1 and 2), which are eradicated now world-wide.
There are still patients that have been affected as the decision to eradicate polio was only enacted in 1988 by the World Health Assembly.
Many Western countries, however, would have been blessedly spared by some of the horrible consequences of these diseases.
Enter, COVID-19 vaccines
The new technologies now are doing something ingenuous – they are providing the instructions, called mRNA, made from generic building blocks (amino-acids – obtained through proteins) to the human host.
This goes into cells, without having the ability to penetrate the nucleus where the hosts’ DNA is stored – this would require a key called nuclear access signal.
Even if it somehow entered the nucleus it would require to be translated into DNA by a tool called reverse transcriptase, the welded into the DNA with another tool called integrase.
The vaccine doesn’t have any of these. So it is strictly impossible to affect the hosts’ DNA.
So this mRNA is being translated by ones’ own protein factory, which ‘read’ the blueprints and synthesize what it codes: the spike protein from the virus, essential in its latching on to the host cells to penetrate and do its mischief.
So the recipient of the vaccine effectively is getting a blueprint for the body to make copies of this protein, which is harmless in itself, as it is made with local building blocks.
The various immune cells floating around, however, recognise this to not be part of the original layout of the host – as a result, the swiftly identify it, tag it and mark it for swift destruction if seen again.
This is also achieved by immune cells called memory cells, which aid in recognising threats to the host.
In short, this is the concept of the Pfizer or Moderna vaccines.
There more than a hundred vaccines being currently prepared world-wide – the other ones in circulation and that have been tested are the AstraZeneca and Jansen ones, which use instead a small benign virus to get introduced in the body carrying these proteins (which it can not use itself) to get the body to do the same as with he mRNA vaccines.
Finally, Novavax is a vaccine which seems to have a high success from a smaller company with high efficiency rate, which uses the older and tried approach of using recombinant proteins (corona viral proteins ones) but with different technology to do so, using non-mammalian cells to produce the proteins, increasing production speed.
What is in the COVID-19 vaccines?
There has been extensive misinformation, about the so-called constituents of the vaccines, with alarmists wanting to spark concerns about the safety of the vaccines.
Any substance introduced into ones’ body, from food to medication, can cause immune reactions.
These new type of vaccines do not even have material of the ‘wild’ virus – it uses the bodies own manufacturing to generate the required component. They have also been extensively tested, and are continuously being tested even now with several ongoing studies.
Most of these vaccines though, operating in tandem and together with how the immune system operates in humans, require a repeat administration to fully unlock their full potential of protection from infection.
The duration of time between vaccinations is important, so getting a booster shot is important to ensure full efficiency of the vaccine.
There are also some logistical consideration – the mRNA technology requires the vaccine to be stored at ultra cold temperatures. Meaning that to get it to certain far-flung locations or a more spread population can be difficult.
The AstraZeneca, on the other hand, can be stored at more conventional and easily obtained temperatures.
The next important question is about whether the vaccine will prevent transmission of the virus.
A recent report out of Israel, where almost 33% of the population has now been vaccinated, hints that the Pfizer vaccine reduces asymptomatic transmission by as much as 60 to 80%.
This has also been found for Moderna and for AstraZeneca.
New trial results are coming out almost daily though – so watch this space.
Another important consideration is about mutation.
This is how these viruses come at us year after year – such as the seasonal flu, despite vaccinations (for the last strains) – as they jump from host to host, they change via mutations.
Which is why they can evade our immune defences, as well as the protections afforded by the vaccines. There are already some new strains of COVID-19, also known as the UK and the South African variants, which are starting to show some differences in how they are made.
The longer populations stay unvaccinated, the more chances the viral strains have to travel from host to host, and the more likely they are to have mutations that may eventually render current vaccines not as effective.
Currently, many of them induce a polyclonal response, which means they generate several antibodies covering several parts of the protein to be recognised. So even several changes will not hamper the vaccines’ efficiency.
A recent study showed with AstraZeneca that it only provides minimal protection against mild to moderate cases of COVID.
But the sooner the population as a whole gets vaccinated, with any vaccine, the more likely it is that the viral transmission will hit roadblocks, which should lead to it receding, just as the Spanish Flu did in 1920.

How do we know which COVID-19 vaccine to take?
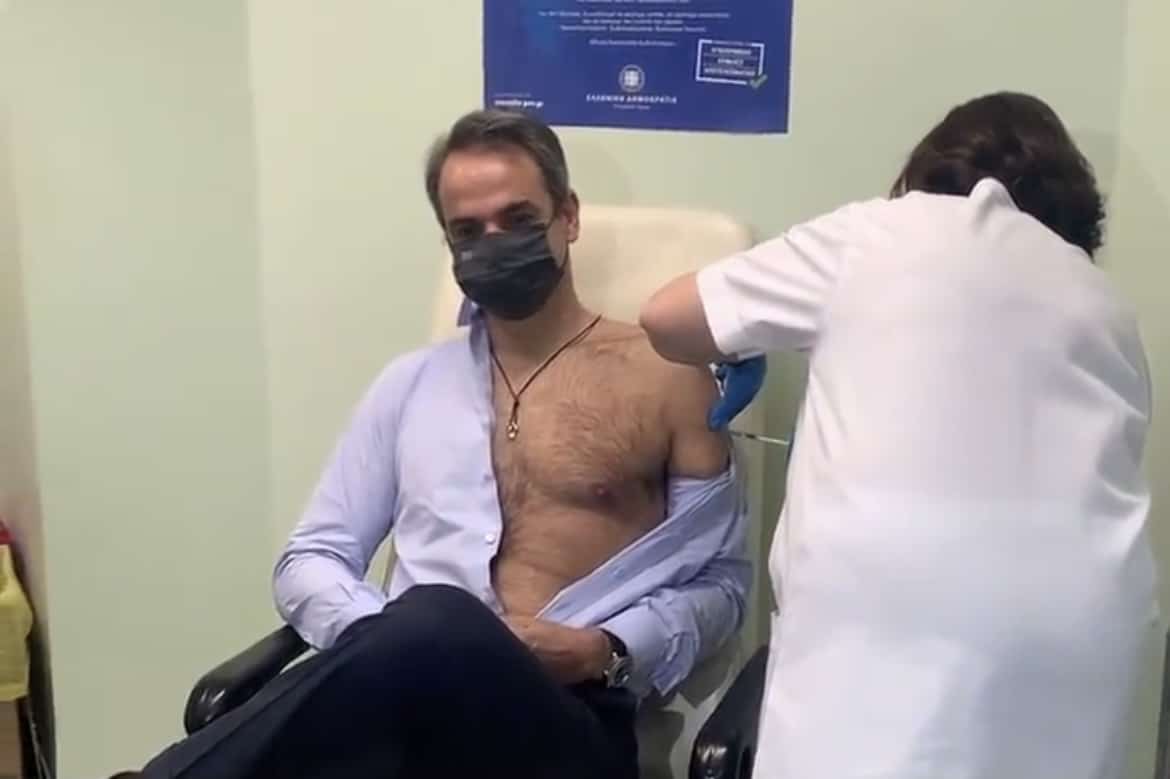
So as this point, with the current state of play, if asked about which one to take, I would suggest that any vaccine on offer should be taken up if made available to you.
Healthcare workers and at risk individuals would, at the moment from what has been released, benefit more from the Pfizer one, and the majority of the population would benefit from the AstraZeneca one.
Will COVID-19 vaccinations be effective?
I believe that the vaccines will be effective in curbing the response and forcing the virus to have a much limited transmission.
Already we have seen a huge decrease across frontline healthcare with the usual colds and smaller viral infections, mostly because people are being more cautious and are more aware of hygiene.
Two winters ago in Australia we had record numbers of influenza and colds presenting through emergencies departments – last year there was an impressive dip and curbing in those. The viruses are endemic – always present, just not given a chance to proliferate as they usually would due to the perceived threat of COVID-19 by the public.
The current vaccines have been tested mostly on individuals aged 16 or older, so advice about giving it to children at this point is unclear – it has been noted, however, that children can be “super-spreaders”, as they can contract it and be relatively unharmed from it, but have an extraordinary capacity to transmit it (particularly when younger).
A more efficient control of this pandemic though, would be in curbing the asymptomatic transmission – so any protection or way of preventing the virus from spreading could yield lasting long term benefits.
Is the end of COVID-19 in sight?
The Spanish Flu lasted about two years.
If predictions hold and vaccination gets delivered on schedule, with adequate uptake, we should see an end to this by the end of this year.
Several airlines have also been looking into vaccination as a prerequisite for boarding international flights.
A return to normal should ensue, but certain institutions and ways of life have been irrevocably changed.
Change can be a force for innovation and new beginnings.
After all, the last pandemic of 1920 resulted in the crazy Twenties…
ABOUT Dr. Nicholas J Lelos
Twitter @DrLelos
LinkedIn: Nicholas Jason Lelos
Medium: doctorlelos
Dr Nicholas Jason Lelos is an American-born doctor of Greek descent, currently residing in Australia, Darwin.
Having undergone all his schooling in the French system, he initially trained as a neuroscientist at the University of Edinburgh in Scotland, and a recipient of a prestigious NATO Fellowship from the Greek government for his work in neuroendocrinology.
Having secured a NHS bursary, he proceeded to study and complete a medicine degree at St George University of London, one of the leading medical establishments of the UK.
He continued to work in London as an internal medicine doctor, with his final rotations being at the world-renowned cancer hospital, the Royal Marsden, having also worked rotations in surgery and general practice.
He was also a trade union representative with the British Medical Association and was a national representative both as a medical student as well as a junior doctor to the Representative body of the organisation.
The next logical step from the experience gathered in this role was to apply and becoming a Medical Practitioner Tribunal Service Panellist with the General Medical Association, the regulatory body of medical practitioners in the UK, both as a Fitness to Practice as well as an Interim Order Panellist, having to adjudicate and determine medicolegal matters pertaining medical practice of peers.
Being a lover of education and learning, he was engaged at running problem-based learning tutorials and being an examiner for his medical school as well as doing a post-graduate degree in Medical Education with University College of London and the Royal College of Physicians.
He also worked as a Viral Challenge Physician in a research capacity for a company called Retroviral, which specialised in the inoculation of quarantined volunteers with the prospect of running tight, rigorous and scientifically sound clinical trials of medications and treatments for viral infections for universities, research groups or private companies.
Having moved over to Australia, he continues to teach at University of Notre Dame, shaping the medical minds of the future, whilst also retraining in Emergency Medicine in South Western Sydney, namely Bankstown, Liverpool and Royal Prince Alfred Hospitals, before moving for a stint to the Canberra Hospital and now currently based at the Royal Darwin Hospital in the Northern Territory.
Representing his peers, he was elected New South Wales representative for his trainee peers in Emergency Medicine, before being chosen as the Trainee Representative Chair for the College of Emergency Medicine until the end of 2019, a role which he pursued vigorously having to travel across Australia and interact with multiple Emergency doctors and departments.
He is still involved in the College, working on reformulating the curriculum and providing better educational material for training.
We warmly welcome Dr. Lelos as a Greek City Times contributor.







